Most read articles
- Page Path
- HOME > Browse articles > Most read articles
Most-read are based on citations from 2024 ~ 2026.
Case Report
- Delayed toxic anterior segment syndrome after cataract surgery: a case report
- Yeoun Sook Chun
- Insights Cataract Refract Surg 2025;10(1):26-31. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.005
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
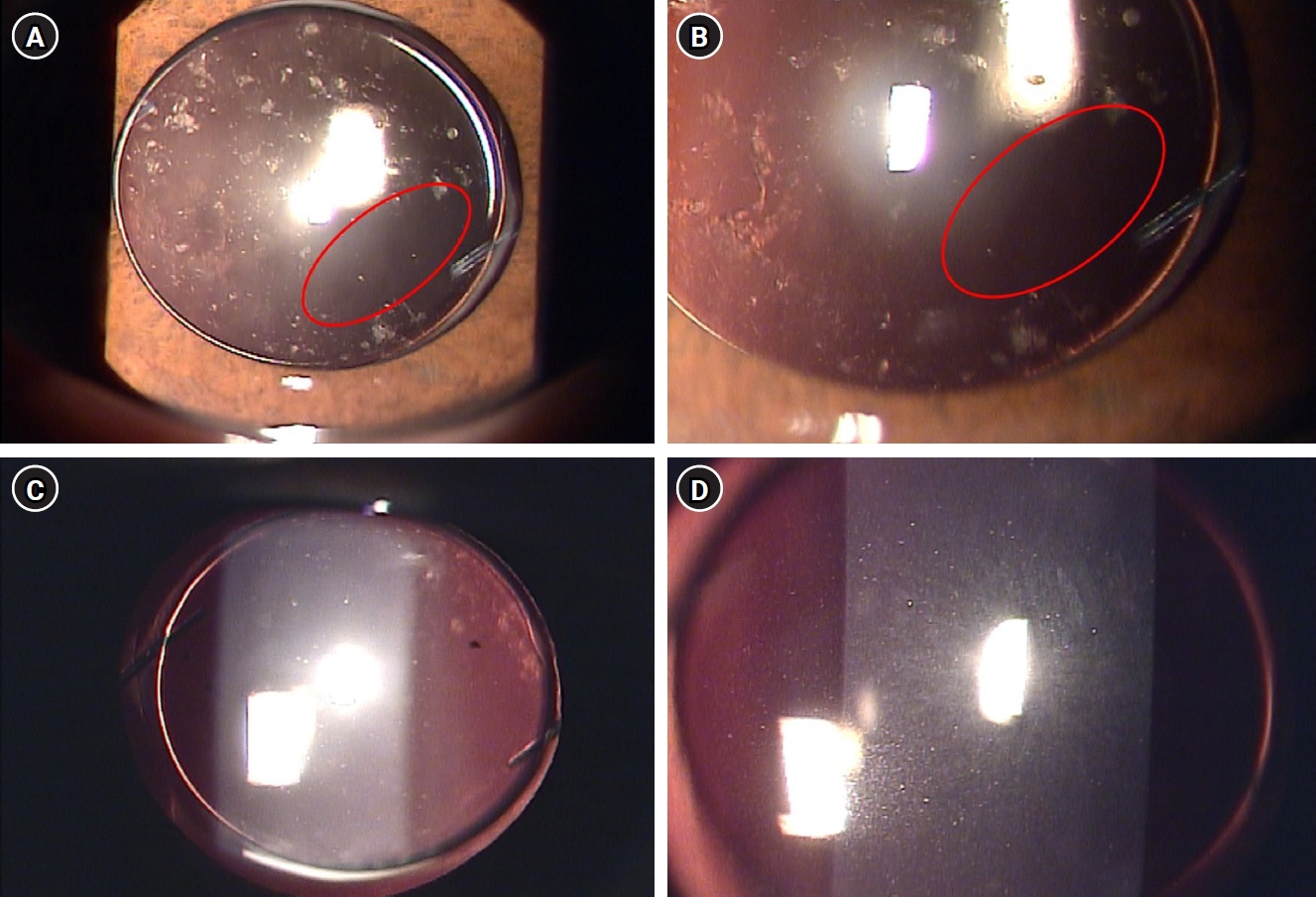
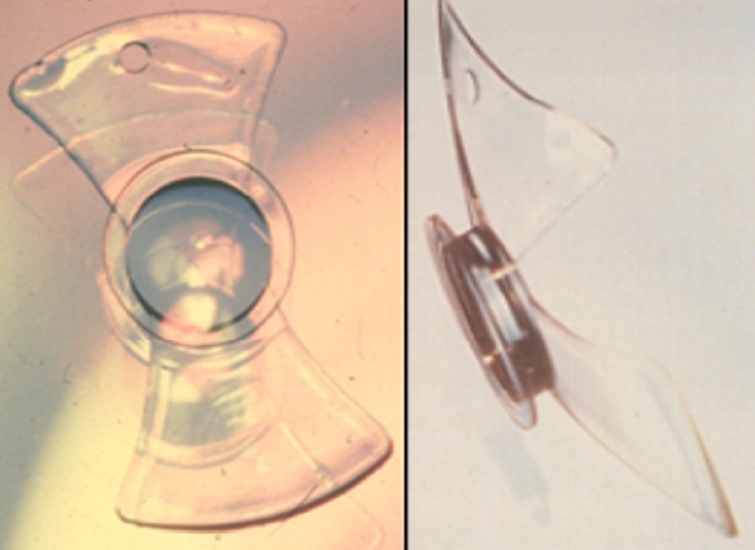
This report describes an unusual case of delayed toxic anterior segment syndrome (TASS) following cataract surgery and its treatment.
Case
summary: A 55-year-old male patient underwent uneventful phacoemulsification with implantation of an intraocular lens (IOL) and eye patching with ophthalmic ointment at the end of the operation. At 1 week postoperatively, a significant increase in the number of anterior chamber inflammatory cells and multiple gray-white deposits on the anterior surface of IOL were noted. All laboratory tests to exclude infectious endophthalmitis were negative. Under the presumptive diagnosis of delayed TASS, an intensive topical steroid was administered. The number of anterior chamber cells decreased; however, the patient complained of blurry vision and multiple whitish precipitates remained on the IOL. Neodymium:yttrium-aluminum-garnet (Nd:YAG) laser treatment was performed to disrupt and remove the precipitates. The deposits were easily and clearly removed using the laser, and there was no recurrence during a 2-year follow-up.
Conclusion
Delayed-onset TASS can manifest as lumpy white inflammatory cell deposits that cannot be controlled with topical steroids. However, Nd:YAG laser treatment can effectively remove inflammatory precipitates.
- 2,411 View
- 28 Download

Editorial
- Personal history of the silicone phakic posterior chamber intraocular lens
- Kenneth J Hoffer
- Insights Cataract Refract Surg 2025;10(1):2-6. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.001
- 2,202 View
- 28 Download

Case Report
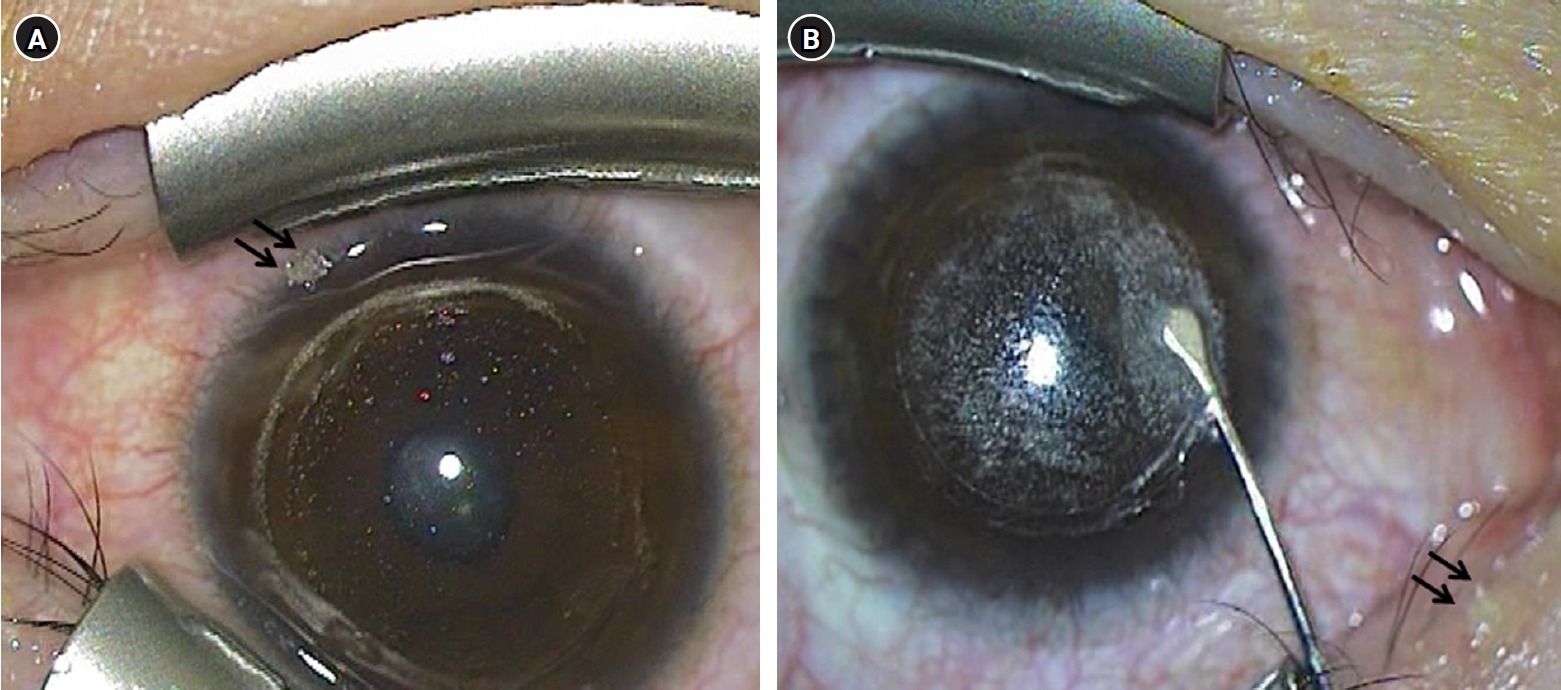
- Diffuse lamellar keratitis after small incision lenticule extraction: presumably related to meibomian gland dysfunction
- Sang Beom Han
- Insights Cataract Refract Surg 2025;10(2):61-64. Published online June 30, 2025
- DOI: https://doi.org/10.63375/icrs.25.008
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This report presents a case of diffuse lamellar keratitis (DLK) after femtosecond laser-assisted small incision lenticule extraction (SMILE). The case was presumably associated with meibomian gland dysfunction (MGD).
Case
summary: A 25-year-old male patient underwent SMILE surgery. Preoperative examination revealed MGD in both eyes. Despite vigorous cleaning of the eyelid margin and irrigation of the ocular surface, meibomian gland secretion floating on the ocular surface was observed after the lenticule extraction in the right eye. At 2 days postoperatively, stage I DLK was detected. After aggressive topical steroid treatment, the DLK completely resolved without any sequalae.
Conclusion
DLK can occur in association with MGD. Attention should be paid when performing SMILE in eyes with MGD.
- 2,126 View
- 17 Download

Original Articles
- Visual and refractive outcomes of keratorefractive lenticule extraction using VISUMAX 800 (SMILE Pro) to correct myopia in Koreans: a 3-month follow-up study
- Sang-Mok Lee, Si-Hoon Park, Tae Keun Yoo, Jae Hyoung Park, Beom Jin Cho, Kee Yong Choi, Jong Woo Kim
- Insights Cataract Refract Surg 2025;10(1):13-18. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.004

-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
The aim of this study was to report the clinical outcomes of SMILE Pro surgery in Korean myopia patients.
Methods
A retrospective analysis was conducted on the medical records of 90 patients (178 eyes) who underwent SMILE Pro surgery at our institution between October 2023 and June 2024 and were followed for 3 months postoperatively.
Results
Preoperative best corrected visual acuity was 0.009±0.020 (logarithm of the minimum angle of resolution). The average spherical equivalent was –5.13±2.16 diopters (range, –1.00 to –10.10 diopters), and the average astigmatism was –1.21±0.91 diopters (range, 0 to –4.0 diopters). Postoperatively, the uncorrected distance visual acuity at 1 day, 1 week, 1 month, and 3 months were 0.061±0.054, 0.013±0.027, 0.009±0.023, 0.005±0.021, respectively. At 3 months postsurgery, the predictive accuracy for spherical equivalent was 100% within ±0.5 diopters and 98.9% within ±0.25 diopters. For astigmatism, the predictive accuracy was 97.2% within ±0.25 diopters and 99.4% within ±0.5 diopters 97.2% and 99.4%. The scores for the efficacy and safety of refractive surgery at 3 months were both 1.01±0.05.
Conclusion
SMILE Pro surgery for myopia correction in Korean patients demonstrated excellent efficacy, safety, and predictive accuracy, with no significant difference compared to conventional SMILE surgery.
- 1,377 View
- 23 Download

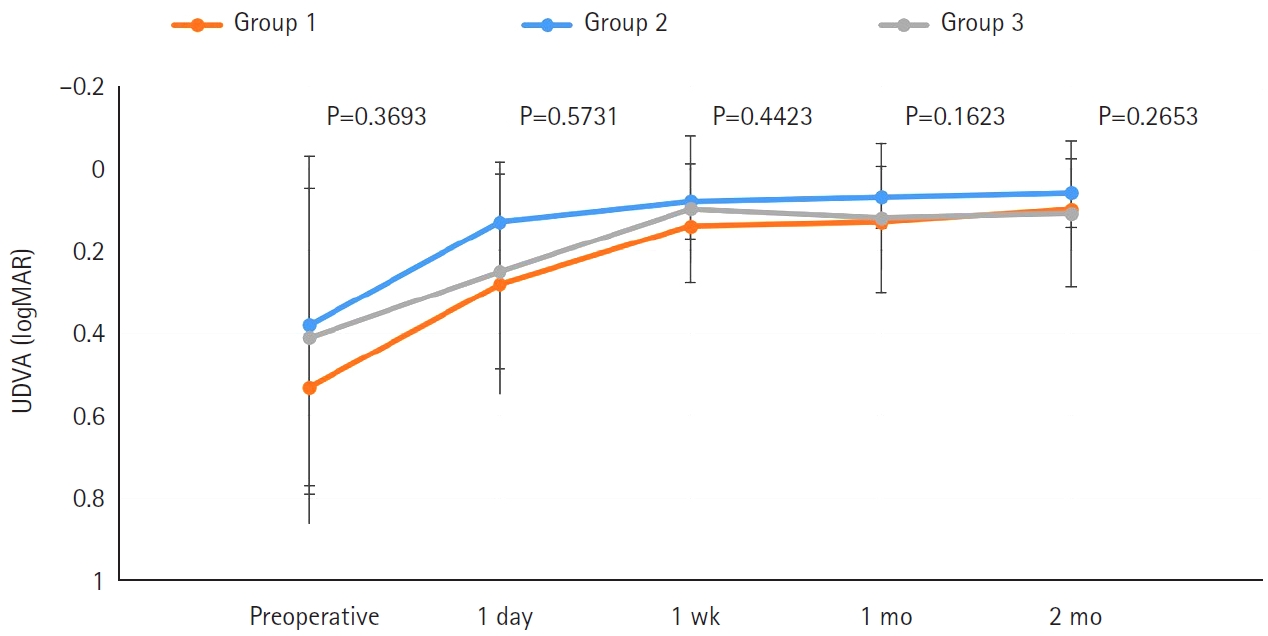
- Efficacy of extended depth of focus, enhanced monofocal, and monofocal intraocular lenses in patients with retinal disease
- Eun Chul Kim
- Insights Cataract Refract Surg 2025;10(2):52-60. Published online June 30, 2025
- DOI: https://doi.org/10.63375/icrs.25.009
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
The aim of this study was to compare the visual quality of extended depth of focus (EDOF), enhanced monofocal, and monofocal intraocular lenses (IOLs) in patients with retinal disease.
Methods
In total, 103 eyes from 93 patients (group 1: enhanced monofocal ICB00, n=36; group 2: EDOF ZXR00, n=36; group 3: monofocal ZCB00, n=31) were retrospectively enrolled. Uncorrected and corrected near visual acuity (UNVA, CNVA), intermediate visual acuity (UIVA, CIVA), and distance visual acuity (UDVA, CDVA), manifest refraction spherical equivalent (MRSE), and satisfaction scores were assessed before and after surgery.
Results
The postoperative UDVA, CDVA, and MRSE of the three groups were better than the preoperative data, respectively (P<0.05). The UIVA of group 1 (0.13±0.12 logMAR) and 2 (0.10±0.11) was significantly better than that of groups 3 (0.25±0.15) (P<0.05). The UNVA of group 2 (0.18±0.12) was significantly better than that of groups 1 (0.32±0.20) and 3 (0.45±0.26; P<0.05). The UDVA of patients with macular edema and macular holes was insignificantly lower than that of epiretinal membranes and high myopia. The overall satisfaction of group 1 (1.58±0.81) and 2 (1.46±0.75) was significantly better than that of groups 3 (1.83±0.97; P<0.05).
Conclusion
EDOF and enhanced monofocal IOLs were associated with better intermediate and near vision than monofocal IOLs in patients with retinal disease. However, monofocal IOLs are recommended in patients with macular edema and macular holes, unlike patients with epiretinal membranes and high myopia.
- 951 View
- 19 Download

Review Articles
- Selection of an optimal intraocular lens according to the stage of epiretinal membrane
- Sang Beom Han
- Insights Cataract Refract Surg 2025;10(1):7-12. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.003
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Epiretinal membrane (ERM), one of the most common retinal diseases, can cause various degrees of visual disturbance, reduced contrast sensitivity, and metamorphopsia. ERM is not infrequently encountered during preoperative evaluations for cataract surgery, and selecting an appropriate intraocular lens (IOL) according to the location and stage of ERM is necessary in order to improve visual outcomes and patients’ satisfaction. This review summarizes the application of various IOLs—such as multifocal, extended depth of focus, and enhanced monofocal IOLs—in eyes with ERM, and discusses the selection of an appropriate IOL.
- 929 View
- 18 Download

- Current updates in the treatment of keratoconus
- Mee Kum Kim
- Insights Cataract Refract Surg 2025;10(2):33-41. Published online June 30, 2025
- DOI: https://doi.org/10.63375/icrs.25.010
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Corneal collagen cross-linking is a primary treatment to slow or halt the progression of keratoconus. For visual rehabilitation, important treatments include contact lenses fitting, intracorneal ring segment implantation, and corneal transplantation. Additionally, either phakic intraocular lenses or corneal therapeutic keratectomy combined with corneal collagen cross-linking can assist in visual rehabilitation with limited indications. New methods for visual rehabilitation, such as stromal keratophakia, have been introduced. This review evaluates and compares the efficacy and safety of various treatments for keratoconus based on the latest information.
- 918 View
- 21 Download

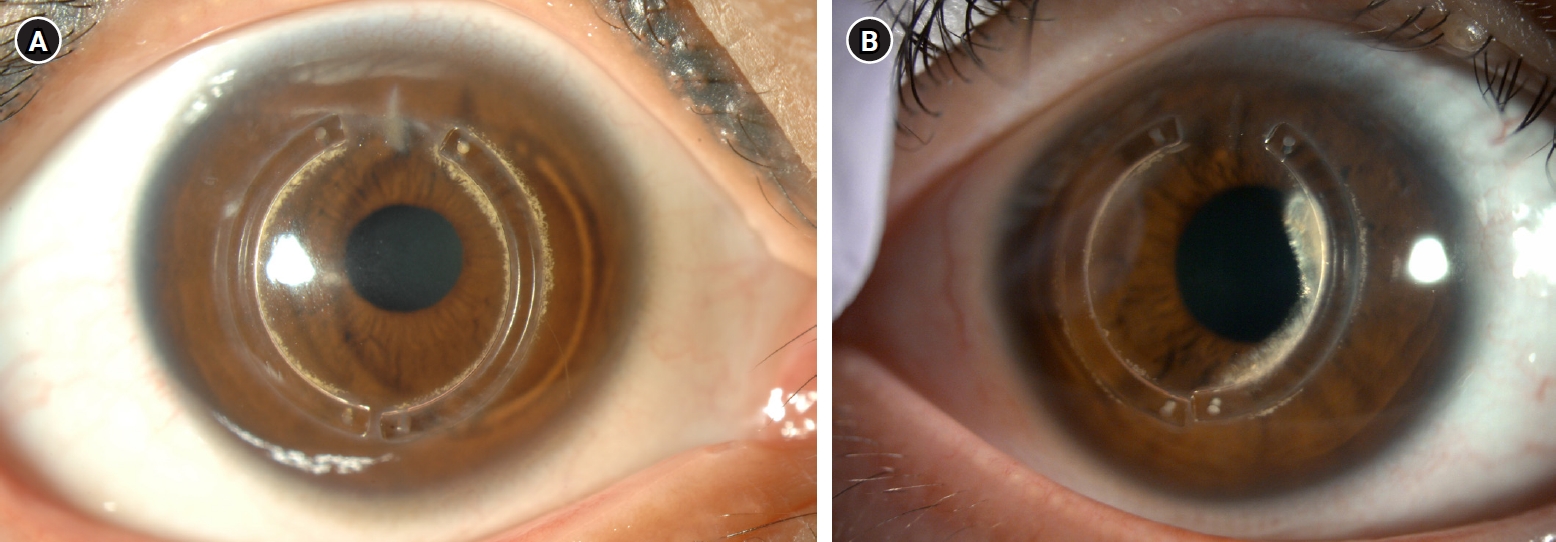
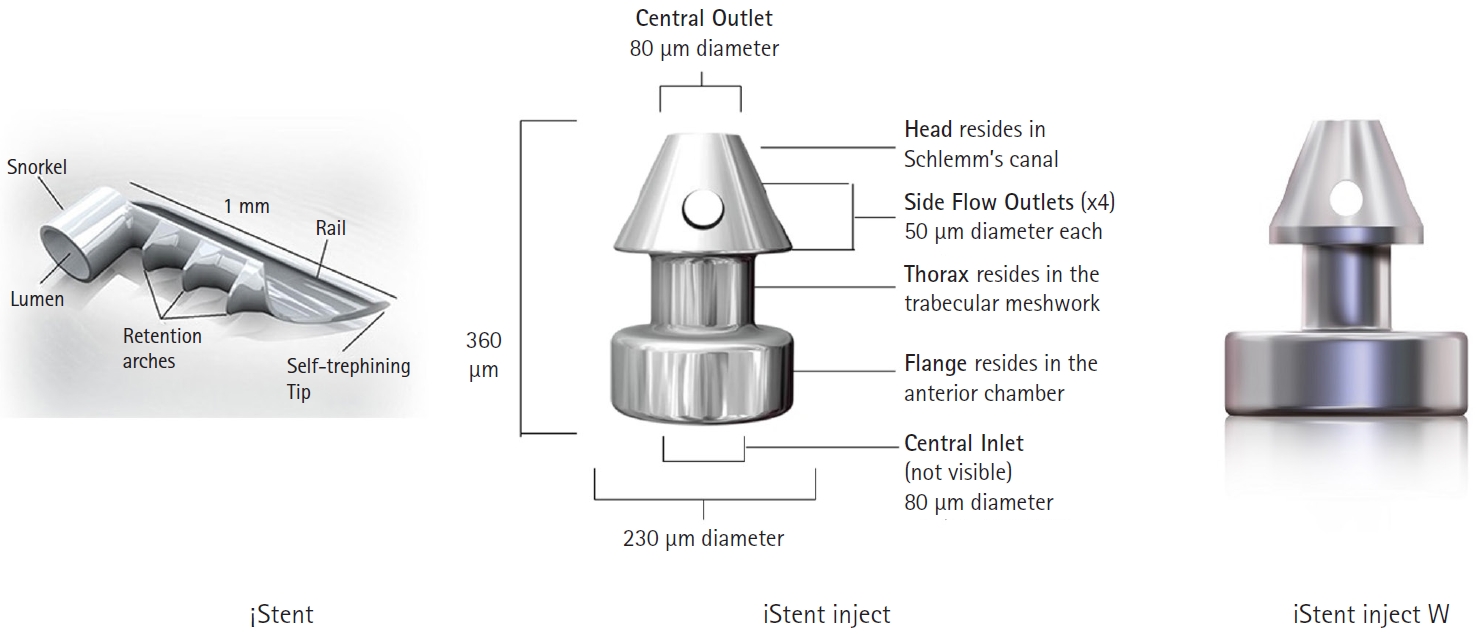
- Trabecular microbypass using iStent combined with cataract surgery
- Yeoun Sook Chun
- Insights Cataract Refract Surg 2025;10(2):42-51. Published online June 30, 2025
- DOI: https://doi.org/10.63375/icrs.25.007
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Minimally invasive glaucoma surgery has revolutionized conventional glaucoma treatment due to its simple procedures, rapid recovery, and few complications. iStent, a trabecular microbypass that can be implanted via combined cataract surgery, has the advantage of lowering intraocular pressure (IOP) independent of bleb formation. Furthermore, it is straightforward to implement and does not involve a substantial burden. iStent has a synergetic effect with phacoemulsification. Combining iStent with phacoemulsification yielded a greater reduction of IOP and glaucoma eyedrops, as well as higher rates of visual field change, than when either modality was used in isolation. iStent has emerged as a new treatment option for patients with mild to moderate glaucoma. This review aims to improve readers’ understanding of iStent by summarizing the surgical techniques needed to correctly insert it for optimal outcomes and discussing problem-solving in the context of patient care.
- 840 View
- 9 Download

Original Article
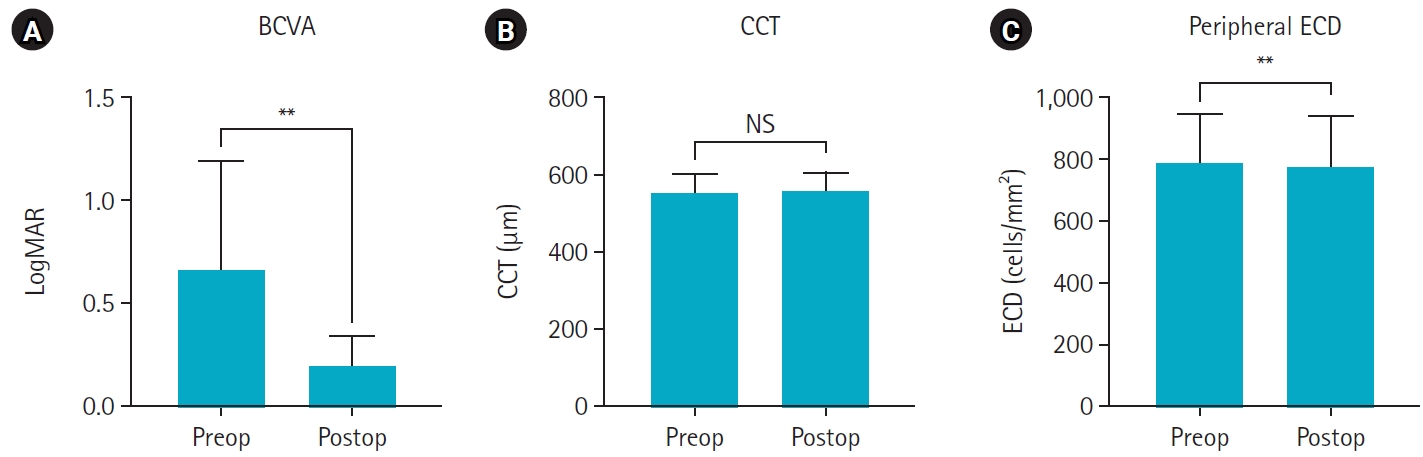
- Clinical manifestations after cataract surgery in patients with moderate Fuchs corneal endothelial dystrophy
- Myung-Sun Song, Dong Hyun Kim
- Insights Cataract Refract Surg 2025;10(1):19-25. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.006
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
The aim of this study was to analyze the clinical outcomes of cataract surgery in patients with moderate Fuchs endothelial corneal dystrophy (FECD) in whom central endothelial cells could not be observed using specular microscopy.
Methods
This retrospective study included nine eyes in seven patients diagnosed with FECD who underwent phacoemulsification at a single institution between January 2023 and November 2024. A single experienced corneal specialist performed slit-lamp examination and phacoemulsification. Best-corrected visual acuity (BCVA), specular microscopy, and central corneal thickness (CCT) measurements were performed preoperatively and postoperatively, and the outcomes were compared.
Results
The mean age of the patients was 69.8±6.5 years. Three were male patients and four were female patients. The mean preoperative CCT was 559.5±51.8 μm and the mean peripheral endothelial cell density was 599.3±129.4 cells/mm2. BCVA significantly improved in all patients postoperatively, with a mean logMAR BCVA improving from 0.65±0.52 preoperatively to 0.19±0.14 postoperatively (P=0.002). The mean CCT showed no significant change (preoperative, 559.6±51.8 μm; postoperative, 566.8±45.1 μm; P=0.218). In patients with follow-up longer than 6 months, an increase in CCT was observed at 30 days postoperatively, but CCT returned to preoperative levels after 90 days.
Conclusion
In patients with moderate-to-severe FECD in whom central endothelial cells cannot be measured, phacoemulsification may provide favorable visual outcomes if peripheral endothelial cells are observed and corneal edema is absent preoperatively.
- 676 View
- 11 Download

Editorial
- Insights in Cataract and Refractive Surgery: a new beginning for a leap forward
- Jong Suk Song
- Insights Cataract Refract Surg 2025;10(1):1-1. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.002
- 577 View
- 12 Download

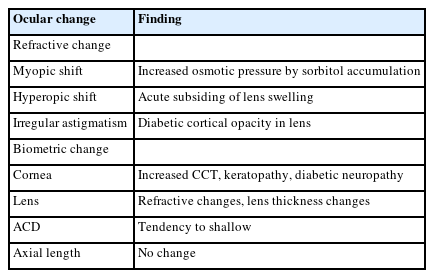
Review Article
- Phacoemulsification in patients with diabetes: from preoperative evaluation to postoperative management
- Yeoun Sook Chun
- Insights Cataract Refract Surg 2025;10(3):65-75. Published online October 31, 2025
- DOI: https://doi.org/10.63375/icrs.25.012
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Diabetes mellitus is one of the most common chronic diseases worldwide and is a leading cause of blindness in patients over the age of 50 years. Patients with diabetes have an elevated risk of developing cataracts compared to individuals without diabetes; furthermore, cataracts also tend to progress more rapidly in this population, leading to the need for surgery at a younger age. This review aims to summarize the key considerations in the management of cataract surgery in patients with diabetes, from preoperative evaluation to postoperative care. Patients with diabetes often present with unstable refractive status, dry eye disease, corneal epithelial defects, and recurrent corneal erosions. They also tend to have reduced corneal endothelial cell density and small pupils, both of which increase the risk of intraoperative complications. Postoperatively, these patients are at risk of developing pseudophakic cystoid macular edema, posterior capsular opacification, endophthalmitis, progression of diabetic retinopathy, and neovascular glaucoma. Patients with long-standing or poorly controlled diabetes face a higher likelihood of postoperative complications, highlighting the importance of regular ophthalmic follow-up examinations. Furthermore, adjunctive treatments such as timely intravitreal injections of anti-vascular endothelial growth factor agents may reduce the risk of vision-threatening complications following cataract surgery.
- 479 View
- 8 Download

Original Articles
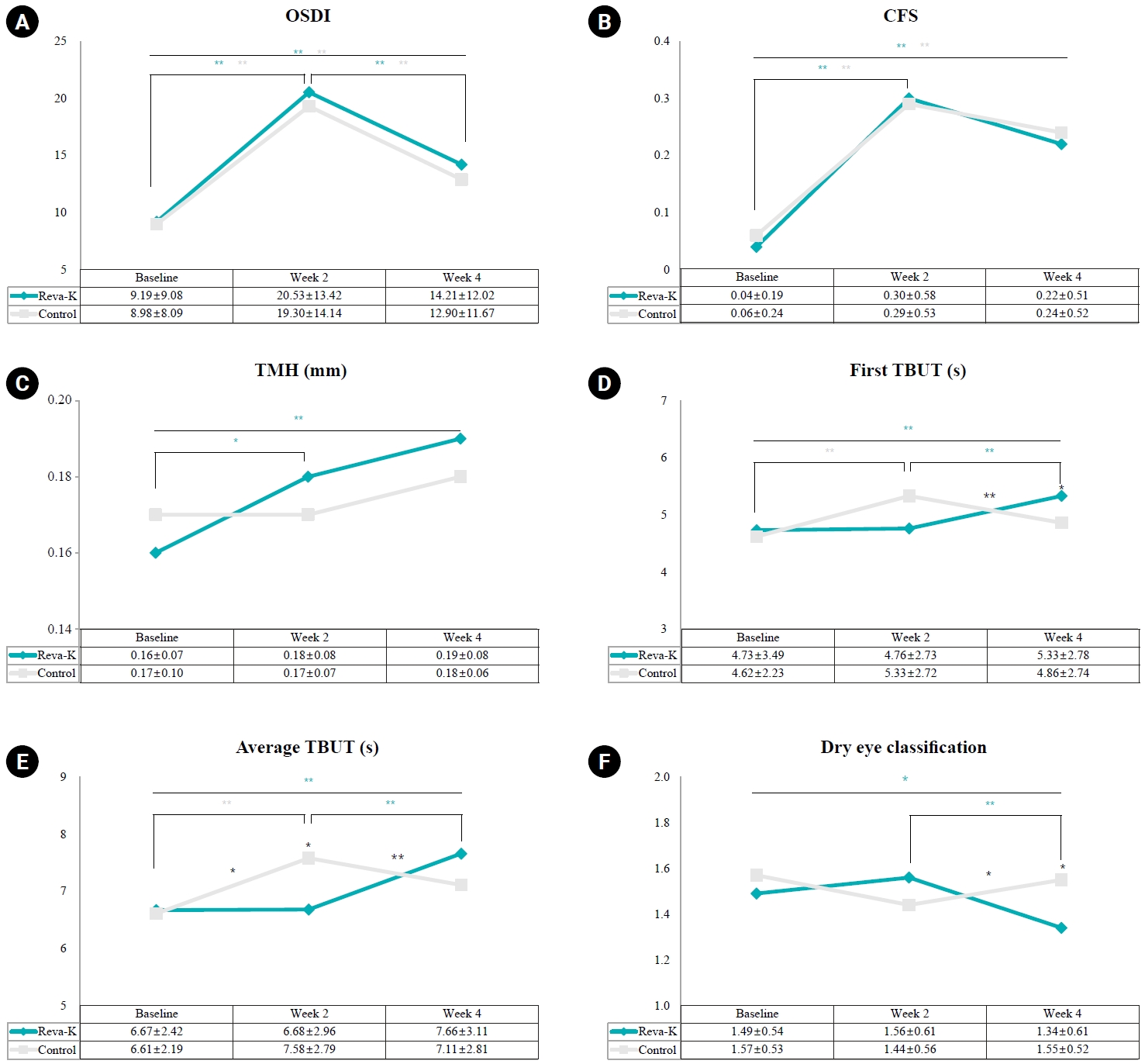
- The effect of 2% rebamipide ophthalmic solution on early dry eye after SMILE surgery: a retrospective study
- Jin Hyoung Kim, Mu Yan Kim, Young A Kwon, Sung Wook Park, Sung Won Byun, Seong Woo Lee, Sung Hyup Lim
- Insights Cataract Refract Surg 2025;10(3):91-102. Published online October 31, 2025
- DOI: https://doi.org/10.63375/icrs.25.013
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
The aim of this study was to investigate the effect of rebamipide 2% ophthalmic solution on early dry eye following small incision lenticule extraction (SMILE) surgery by analyzing dry eye indicators before and after the procedure.
Methods
In this retrospective study, an initial sample of 372 SMILE surgery patients were divided into a rebamipide group (artificial tears and 2% rebamipide) and a control group (artificial tears only). Changes in dry eye indicators, including the Ocular Surface Disease Index (OSDI), corneal fluorescein staining (CFS) score, tear meniscus height (TMH), tear break-up time (TBUT), and dry eye classification, were analyzed at 2 and 4 weeks postoperatively in comparison with the preoperative baseline.
Results
In total, 250 patients (250 eyes) were selected: 135 in the rebamipide group and 115 in the control group. Preoperative characteristics such as gender, age, spherical equivalent refraction, ablation depth, and optical zone size showed no significant differences between the two groups. Both groups demonstrated a significant increase in OSDI and CFS scores at 2 weeks postoperatively, followed by a decrease at 4 weeks, with no significant differences between groups. TMH increased significantly in the rebamipide group at 2 and 4 weeks (P=0.043, P=0.004), but showed no significant change in control group or intergroup difference. No significant difference was found in the first TBUT between the two groups at any time point, but the average TBUT significantly and rapidly increased from 2 to 4 weeks postoperatively in the rebamipide group (P=0.001). The dry eye classification was significantly lower in the rebamipide group at 4 weeks postoperatively (P=0.014).
Conclusion
The use of rebamipide 2% ophthalmic solution immediately after SMILE surgery is expected to be helpful in treating early postoperative dry eye, as it increased TMH and TBUT starting from 2 weeks postoperatively.
- 457 View
- 8 Download

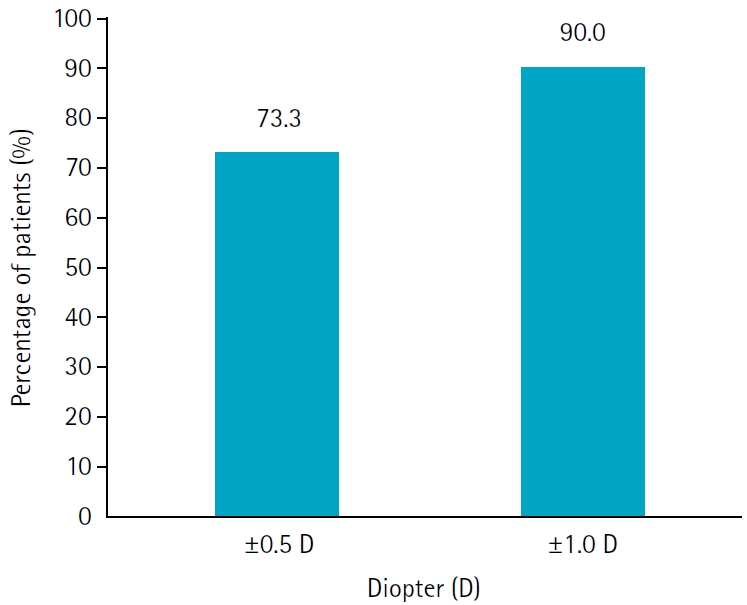
- Results of multifocal intraocular lens implantation in patients who underwent corneal refractive surgery
- Eun Chul Kim
- Insights Cataract Refract Surg 2025;10(3):76-82. Published online October 31, 2025
- DOI: https://doi.org/10.63375/icrs.25.011
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
The aim of this study was to evaluate the clinical results of multifocal intraocular lenses in patients who underwent corneal refractive surgery.
Methods
Thirty eyes (16 patients; Synergy: ZFR00V) were retrospectively enrolled. Uncorrected and corrected near visual acuity (UNVA, CNVA), intermediate visual acuity (UIVA, CIVA), and distant visual acuity (UDVA, CDVA), manifest refraction spherical equivalent (MRSE), and satisfaction score were assessed before and after surgery.
Results
The postoperative UDVA, UIVA, UNVA, and MRSE of the three groups exhibited improvements compared to the preoperative data (P<0.05). The error between the postoperative refraction and the intraocular lens calculation was smaller with the Barrett True K formula than with the Haigis-L formula (P<0.05). The defocus curve at 0 diopter (D) increased, from –1 to –1.5 D, and from –2.5 to –4.0 D, indicating improved vision at distant, intermediate, and near distances. Distance satisfaction (1.47±0.63), near satisfaction (1.25±0.71), and overall satisfaction (1.36±0.42) were good, but light scattering and halo satisfaction (1.97±0.85) yielded a poor result.
Conclusion
In patients with cataracts who underwent corneal refractive surgery, multifocal intraocular lens implantation resulted in excellent uncorrected visual acuity at distant, intermediate, and near distances. However, careful consideration should be given to patient selection due to the incidence of side effects such as glare and halos.
- 331 View
- 10 Download

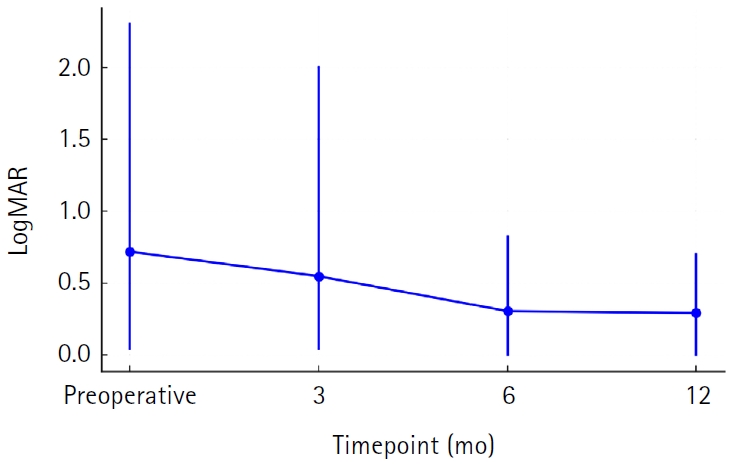
- Clinical results of combined Descemet membrane keratoplasty and cataract operation (triple Descemet membrane keratoplasty) from imported donor corneas: a retrospective study
- Hyung Keun Lee, Sung Soo Kang, Jin Suk Chun, So Young Kim, Dong Ihll Lee
- Insights Cataract Refract Surg 2025;10(3):83-90. Published online October 31, 2025
- DOI: https://doi.org/10.63375/icrs.25.014
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study reports the clinical outcomes, after triple Descemet membrane endothelial keratoplasty (DMEK) performed using imported corneas.
Methods
A retrospective study was conducted on 30 eyes of 26 patients who underwent Descemet's membrane keratoplasty concurrently with cataract surgery, referred to as triple DMEK, from January 2023 to June 2025. After routine preoperative examinations for keratoplasty as well as cataract surgery, uneventful DMEK surgery was performed concurrently with cataract surgery. All patients visited the clinic at 1, 3, 6, and 12 months after surgery to observe changes, including uncorrected and best spectacle corrected visual acuity, refractive error, corneal thickness, and endothelial cell density.
Results
Preoperatively, 12 of the 30 eyes had Fuchs corneal endothelial dystrophy and 12 had endothelial failure following phakic intraocular lens implantation. The average observation period for the subjects was 437±263 days. After triple DMEK surgery, the patients' uncorrected visual acuity gradually improved from 0.73±0.6 (logMAR) before surgery to 0.65±0.54 at 3 months and 0.29±0.26 at 1 year (P<0.001). The change in corneal thickness was 565.7±70.0 μm before surgery, 535.2±44.2 μm at 3 months after surgery, 549.7±73.5 μm at 6 months, and 535.82±49.0 μm at 12 months, but no statistical significance was found compared to before surgery at any time point (P>0.05). The endothelial cell density was 798±363 cells/mm2 before surgery, 1,479±475 cells/mm2 at 3 months after surgery, 1,456±456 cells/mm2 at 6 months, 1,332±346 cells/mm2 at 12 months, and 1,399±519 cells/mm2 at the last visit (P<0.001).
Conclusion
Triple DMEK surgery, which is performed for various corneal diseases, is relatively safe. No significant endothelial damage, refractive changes, or visual acuity abnormalities were observed up to one year after surgery. Future prospective studies including a larger number of participants are warranted to evaluate the safety and clinical outcomes of triple DMEK using imported corneas.
- 251 View
- 3 Download


 KSCRS
KSCRS
 First
First Prev
Prev


