Funded articles
- Page Path
- HOME > Browse articles > Funded articles
Original Article
- Clinical results of combined Descemet membrane keratoplasty and cataract operation (triple Descemet membrane keratoplasty) from imported donor corneas: a retrospective study
- Hyung Keun Lee, Sung Soo Kang, Jin Suk Chun, So Young Kim, Dong Ihll Lee
- Insights Cataract Refract Surg 2025;10(3):83-90. Published online October 31, 2025
- DOI: https://doi.org/10.63375/icrs.25.014
- Funded: National Research Foundation of Korea, Ministry of Education, Science, and Technology
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study reports the clinical outcomes, after triple Descemet membrane endothelial keratoplasty (DMEK) performed using imported corneas.
Methods
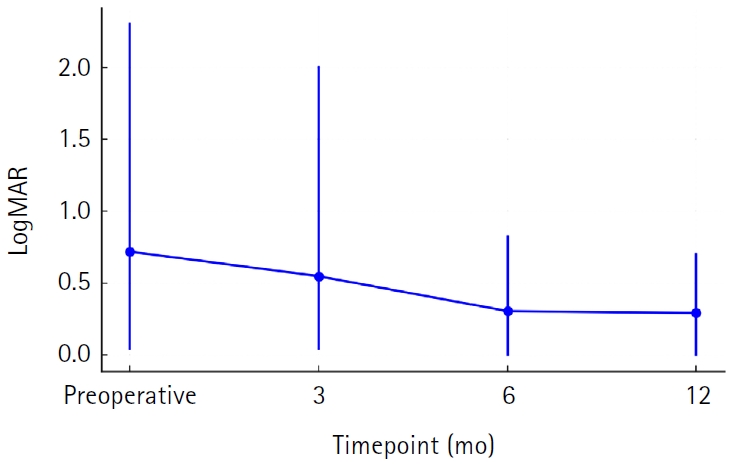
A retrospective study was conducted on 30 eyes of 26 patients who underwent Descemet's membrane keratoplasty concurrently with cataract surgery, referred to as triple DMEK, from January 2023 to June 2025. After routine preoperative examinations for keratoplasty as well as cataract surgery, uneventful DMEK surgery was performed concurrently with cataract surgery. All patients visited the clinic at 1, 3, 6, and 12 months after surgery to observe changes, including uncorrected and best spectacle corrected visual acuity, refractive error, corneal thickness, and endothelial cell density.
Results
Preoperatively, 12 of the 30 eyes had Fuchs corneal endothelial dystrophy and 12 had endothelial failure following phakic intraocular lens implantation. The average observation period for the subjects was 437±263 days. After triple DMEK surgery, the patients' uncorrected visual acuity gradually improved from 0.73±0.6 (logMAR) before surgery to 0.65±0.54 at 3 months and 0.29±0.26 at 1 year (P<0.001). The change in corneal thickness was 565.7±70.0 μm before surgery, 535.2±44.2 μm at 3 months after surgery, 549.7±73.5 μm at 6 months, and 535.82±49.0 μm at 12 months, but no statistical significance was found compared to before surgery at any time point (P>0.05). The endothelial cell density was 798±363 cells/mm2 before surgery, 1,479±475 cells/mm2 at 3 months after surgery, 1,456±456 cells/mm2 at 6 months, 1,332±346 cells/mm2 at 12 months, and 1,399±519 cells/mm2 at the last visit (P<0.001).
Conclusion
Triple DMEK surgery, which is performed for various corneal diseases, is relatively safe. No significant endothelial damage, refractive changes, or visual acuity abnormalities were observed up to one year after surgery. Future prospective studies including a larger number of participants are warranted to evaluate the safety and clinical outcomes of triple DMEK using imported corneas.
- 252 View
- 3 Download

Case Report
- Diffuse lamellar keratitis after small incision lenticule extraction: presumably related to meibomian gland dysfunction
- Sang Beom Han
- Insights Cataract Refract Surg 2025;10(2):61-64. Published online June 30, 2025
- DOI: https://doi.org/10.63375/icrs.25.008
- Funded: National Research Foundation of Korea, Ministry of Education
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
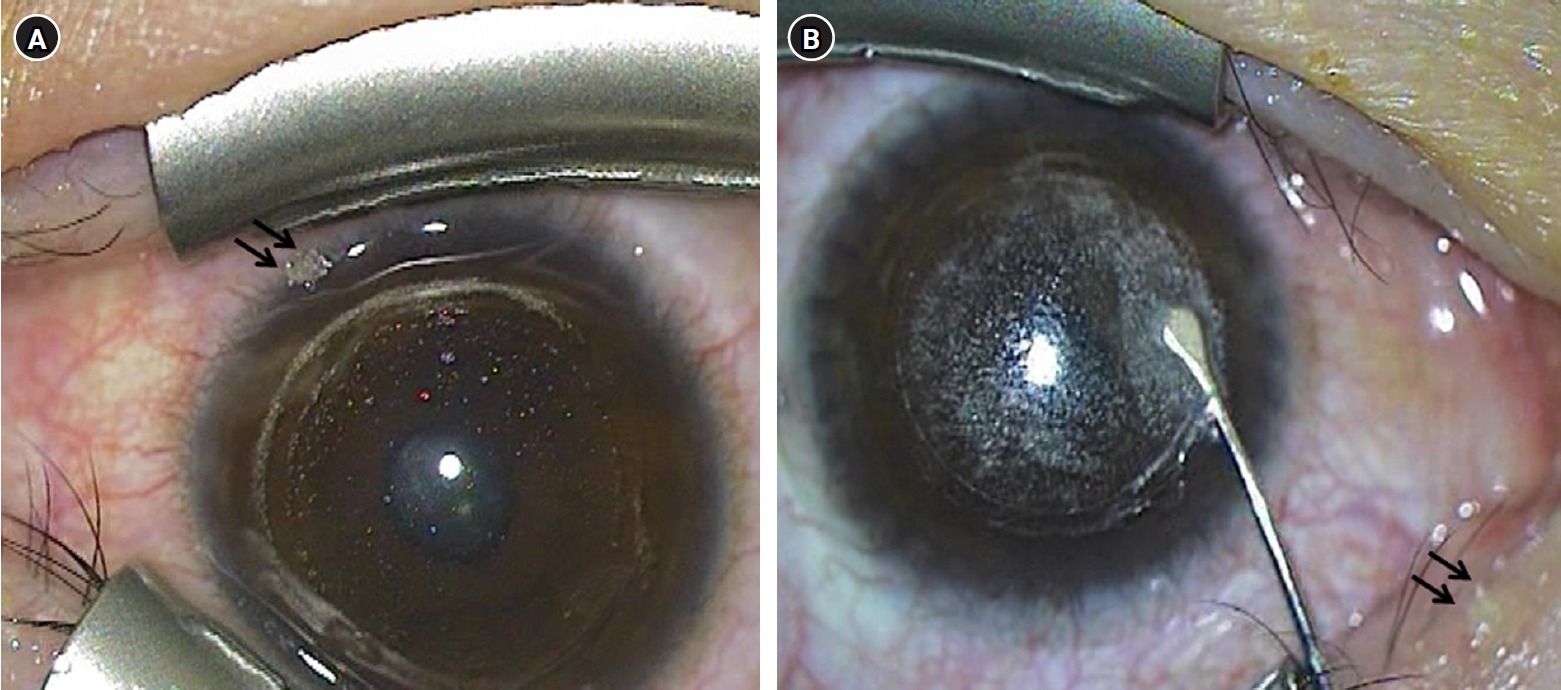
This report presents a case of diffuse lamellar keratitis (DLK) after femtosecond laser-assisted small incision lenticule extraction (SMILE). The case was presumably associated with meibomian gland dysfunction (MGD).
Case
summary: A 25-year-old male patient underwent SMILE surgery. Preoperative examination revealed MGD in both eyes. Despite vigorous cleaning of the eyelid margin and irrigation of the ocular surface, meibomian gland secretion floating on the ocular surface was observed after the lenticule extraction in the right eye. At 2 days postoperatively, stage I DLK was detected. After aggressive topical steroid treatment, the DLK completely resolved without any sequalae.
Conclusion
DLK can occur in association with MGD. Attention should be paid when performing SMILE in eyes with MGD.
- 2,127 View
- 17 Download

Review Article
- Selection of an optimal intraocular lens according to the stage of epiretinal membrane
- Sang Beom Han
- Insights Cataract Refract Surg 2025;10(1):7-12. Published online February 28, 2025
- DOI: https://doi.org/10.63375/icrs.25.003
- Funded: National Research Foundation of Korea, Ministry of Education
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Epiretinal membrane (ERM), one of the most common retinal diseases, can cause various degrees of visual disturbance, reduced contrast sensitivity, and metamorphopsia. ERM is not infrequently encountered during preoperative evaluations for cataract surgery, and selecting an appropriate intraocular lens (IOL) according to the location and stage of ERM is necessary in order to improve visual outcomes and patients’ satisfaction. This review summarizes the application of various IOLs—such as multifocal, extended depth of focus, and enhanced monofocal IOLs—in eyes with ERM, and discusses the selection of an appropriate IOL.
- 929 View
- 18 Download


 KSCRS
KSCRS
 First
First Prev
Prev


